Coding and Classification in the Pacific:
Why Clinical Coding and Continuing
Education is Important
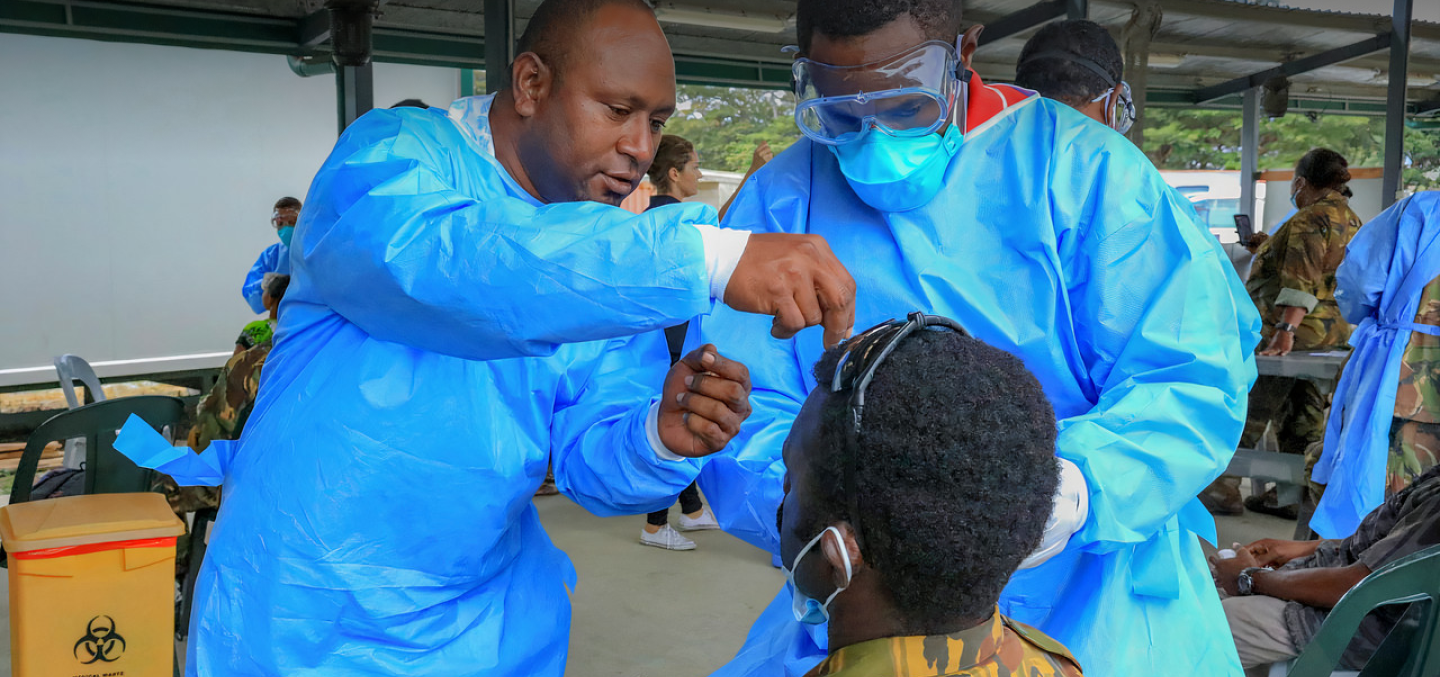
Health care workers have a professional responsibility to stay current with their education. This includes access to continuing education with the latest clinical coding updates. With the need to have better information to make better decisions for better healthcare, the growing number of diagnosis codes and the need to apply these codes accurately is now more important than ever.
The International Statistical Classification of Diseases 10th Edition (ICD-10) is a globally adopted coding tool used to standardise the collection of health information for epidemiology, health management and clinical purposes. The classification is maintained by the World Health Organization (WHO). ICD-10 has been designed to promote international comparability in the collection, processing and presentation of morbidity and mortality statistics. As a result, this is the quintessential reference used worldwide for mortality coding to accurately establish the underlying cause of death, and for morbidity coding to record the patient’s main condition during an episode of care. Some countries (such as Australia among many others) have developed ICD-10 modifications and accompanying procedure classifications to better capture specific diseases, medical and surgical interventions. These additions provide better insights on healthcare episodes to facilitate better program planning and decision making.

The integrity of a country’s health information requires standardized and accurate clinical coding based on complete and accurate hospital medical records and death certificates. The positive outcomes are unquestionable. This includes producing quality information in a standardized way with high coverage that can be used by governments, researchers and NGOs to formulate public health policies, interventions and programs aimed at improving the health of a nation. Therefore, for Pacific countries that have adopted clinical coding to support the provision of data to manage healthcare, well-trained morbidity and mortality coders has proved to yield the greatest value.
The next edition of the international disease classification is ICD-11. It is scheduled for international implementation commencing in January 2022. It will be accompanied by a procedure classification termed ICHI. ICD-11 has almost 5 times more codes than ICD-10. Therefore, establishing a solid education foundation in the Pacific is now much more important to support the transition to the updated classifications in the future. Furthermore, as medical knowledge advances, new diseases emerge and health information systems become more sophisticated such as adopting artificial intelligence, there will be a need to continually update the ICD. By moving to ICD-11, countries will be in a much better position to take advantage of these new capabilities and features in the future.
PHIN is working collaboratively with the Brisbane Accord Group (BAG), the Queensland University of Technology (QUT), the Pacific Community (SPC) and WHO in improving the clinical coding capabilities in the Pacific region. Furthermore, PHIN is exploring academic partnership opportunities with the Fiji National University (FNU) to provide continuing education for clinical coders for Pacific countries.
PARTNERS
PROJECT TYPE
LOCATION
SHARE
RELATED RESOURCES

MATERIAL MAY 2019
WHO: International Statistical Classification of Diseases and Related Health Problems (ICD)
VIEW MATERIAL
MATERIAL JULY 2019
ICD-10-AM/ACHI/ACS
VIEW MATERIAL
MATERIAL MAY 2019
WHO: ICD-11 Implementation or Transition Guide
VIEW MATERIAL
MATERIAL NOVEMBER 2020
Introduction To Coding And Classification In The Pacific - Icd-10-am And Snomed Ct-au (4 November 2020)
WATCH THE VIDEO